Limits of Interpreting A Drug Test
Showing: Forensic Technology

There are many variables regarding the analyses of substance abuse testing. Clients will often ask about specifics pertaining to the determination of time, dose and frequency when detecting substance(s) of abuse.
When testing a reservoir matrix- a material or substance which can accumulate and retain drug and alcohol biomarkers (eg., urine, blood, hair, nail, umbilical cord, or meconium, etc.), the reported quantitation of a drug or its metabolite cannot be used to determine when/if a specific substance was used, how much of a substance was used or how often a substance was used. Test results show only if a substance was detected or not detected.
A specimen’s window of detection provides an estimated timeframe for detecting substance(s) of abuse. Based on extensive research studies, the generally accepted windows of detection for specimens used in our testing are as follows:
- Scalp Hair- Up to approximately 3 months prior to collection.
- Fingernail- Up to approximately 3-6 months prior to collection.
- Umbilical Cord- Up to approximately 20 weeks prior to birth.
- Meconium- Up to approximately 20 weeks prior to birth.
- Urine- Up to approximately 2-3 days prior to collection.
- Blood (PEth)-May be up to approximately 2-4 weeks prior to collection.
It is important to know that the interpretation of drug testing results may be determined by a Medical Review Officer (MRO). A Medical Review Officer is a licensed physician (MD or DO) who has knowledge of substance abuse disorders and has the appropriate medical training to interpret and evaluate an individual’s positive test result together with his or her medical history and any other relevant biomedical information.1This is an incredibly important aspect of drug testing. A laboratory can detect substances, but an MRO may be used to interpret what that detection means.
1. Journal of Occupational and Environmental Medicine: (January 2003-Volume 45-Issue 1-p 102-103) Qualifications of Medical Review Officers (MRO’s) in Regulated and Nonregulated Drug Testing. Departments: ACOEM Consensus Opinion Statement
What you need to know about meconium collection.
by Michelle Lach, MSIMC
Meconium is the first stool of a newborn infant. It is produced in utero and consists of materials such as epithelial cells, bile, mucous, and more. In most newborns, meconium is generally passed in the first day or so of life, has no odor, and appears as a very dark, tar-like substance. This helps distinguish meconium from the next phase of passage called transitional stool.
Transitional stool will start to have an odor and present with a more brown, green, or yellow color as the newborn starts digesting milk. When drug testing the meconium of a newborn, it is important to note this difference since only meconium is created during gestation and transitional stool is created after birth. Collection of any stool other than meconium for drug testing purposes may result in a rejected specimen.
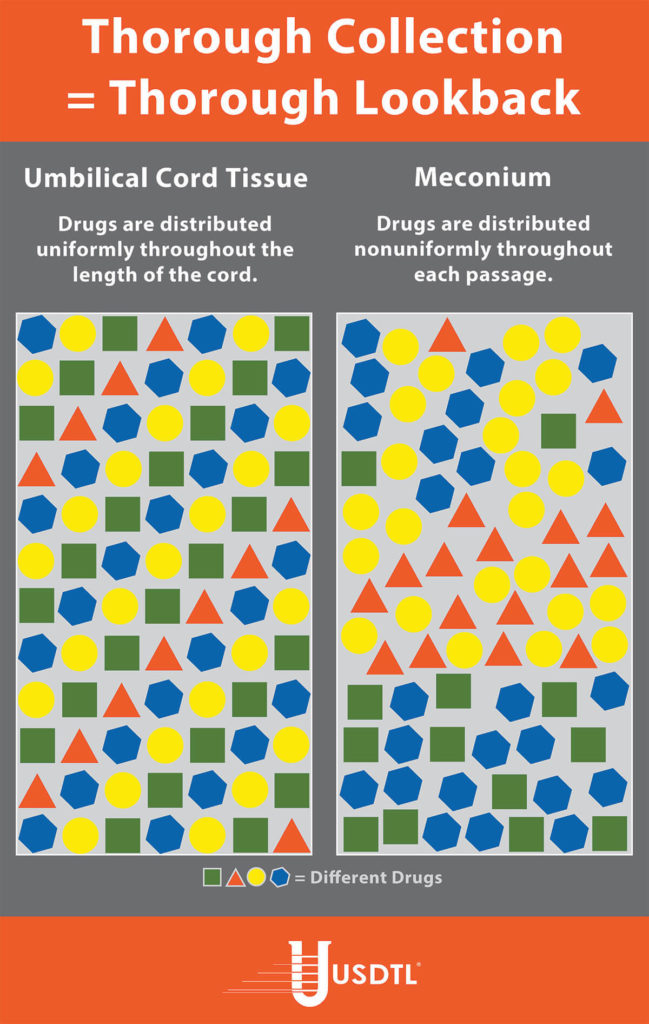
Unlike umbilical cord tissue, drugs are not distributed uniformly throughout the meconium specimen (see Figure 1). Because of this, the collection of the entire mass of meconium is highly encouraged to assure that there will be enough specimen to test, and that the maximum window of drug detection is achieved. It can take multiple passages of meconium before the newborn begins the transitional stool phase.
We require a minimum of 3 grams of meconium to be able to properly run our tests, so collecting the entire passage of meconium from newborns that have been exposed to substances of abuse is highly critical since they tend to have lower birth weights and create less specimen in the first place. If there is not enough specimen to run the test, the results are reported out as QNS. Quantity Not Sufficient (QNS) is a result of not having a sufficient quantity (volume) of specimen to test for the panels ordered.
What You Need To Know: Testing for Drug Exposure vs. Ingestion
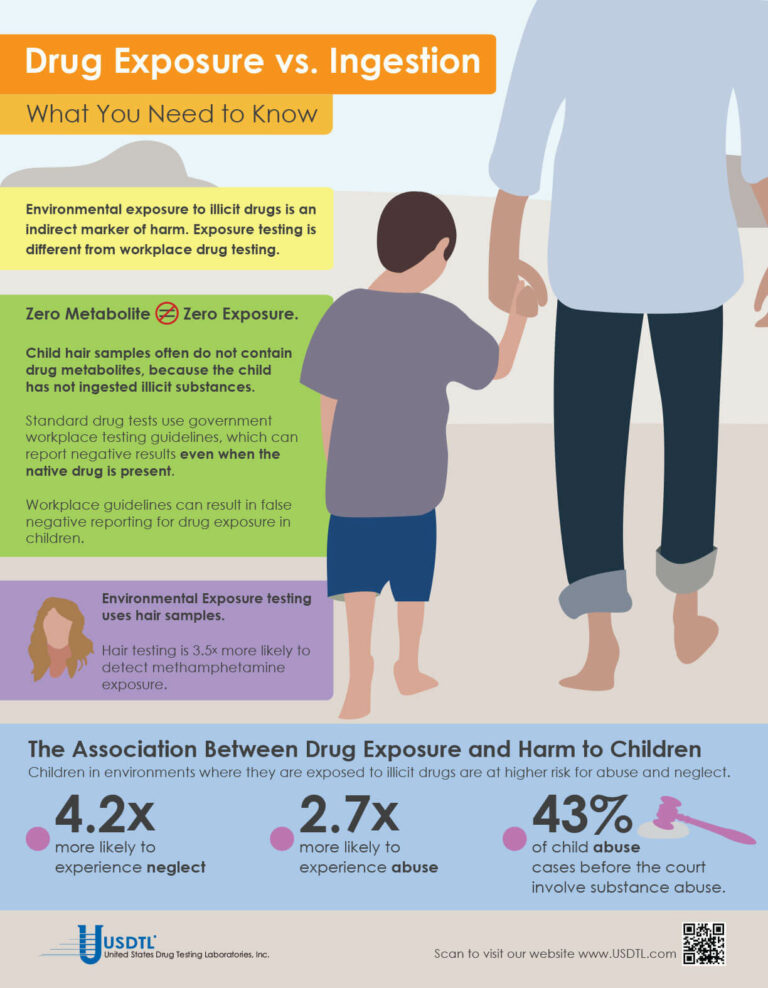
Testing for environmental exposure to illicit drugs is a powerful tool for protecting the welfare of children. Exposure testing is different from typical drug testing, and when properly done, has the potential to reduce the risk of harm to children.
No Metabolite Does NOT Mean No Exposure
Testing labs often apply government workplace testing guidelines to child exposure testing samples. Under workplace guidelines, negative results are reported when drug metabolites are absent in the testing sample, even if the native drug is present.
Child hair and nail samples for exposure testing often do not contain drug metabolites because the child has not ingested illicit substances. Adhering to workplace guidelines can result in false negative reporting for drug exposure, especially when children are involved.
Environmental Exposure
Environmental Exposure testing is most effective in alternative sample types, such as hair and fingernails. For example, hair testing is 3.5x more likely to detect methamphetamine exposure than urine testing. Typical drug testing samples are washed to remove drug biomarkers resulting from exposure. Environmental exposure testing eliminates this step.
– Click here to download the pdf.
When a child is exposed to illegal substance abuse they often also face other coexisting obstacles to a normal life – neglect, abuse, violence, and other vulnerabilities. Substance abuse is a disease, one that often prevents adults from doing what is in a child’s best interests. Our environmental exposure test for children can help.
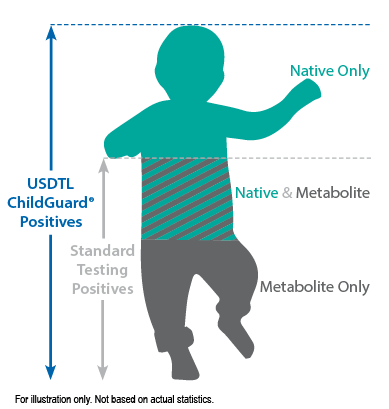
Our hair environmental exposure test is the only drug test designed to detect passive exposure to drugs and detect both native drugs and drug metabolites in the hair specimen. Drug metabolites are produced in the body only if drugs have been ingested. Children in drug exposed environments are most often not drug users themselves, so drug metabolites are typically absent in child specimens. However, the hair, like a sponge, can absorb non-metabolized drug (native drug) if it is exposed through things such as touching or being in contact with drugs or drug users.
Standard hair tests with other labs will only report a positive exposure result if drug metabolites are detected, even when the native drug is in the child’s hair specimen. Our hair environmental exposure test reports a positive result if either native drugs or drug metabolites are detected.
A hair exposure test can provide evidence of drugs in a child’s environment for the past 3 months. A positive test result suggests that the child has experienced one or more of the following: passive inhalation of drug smoke, contact with drug smoke, contact with sweat or sebum (skin oil) of a drug user, contact with the actual drug, or accidental or intentional ingestion of illegal drugs.
ChildGuard®is the only child hair test designed to detect exposure to native drugs and drug metabolites.
Please click here to read the full article by Eric Frazer, Ph. D., and Linda Smith, Ph. D., in our Fall issue of Substance.
One of the most common issues that arises in Juvenile and Family Court is parental substance abuse. Once this allegation has been raised, there is immediate concern about the child’s safety and well-being. In particular, there is often concern about neglect and abuse. For example, will the parent prioritize drug seeking over caring for the child? Will the parent drive under the influence, with the child in the vehicle? Less commonly mentioned in the courtroom, especially in the family courtroom, is potential child exposure to drugs. Unfortunately, this is a significant risk to children, and should be considered and discussed in every case.
One of the challenges family lawyers and courts face is how to properly investigate the substance abuse allegation and determine if it is a valid concern. Gathering and organizing the most relevant information has historically been difficult to do because of a lack of awareness regarding what is most relevant and important. Fortunately, the drug testing lab can bridge that gap of uncertainty, especially when there is an allegation about child exposure.
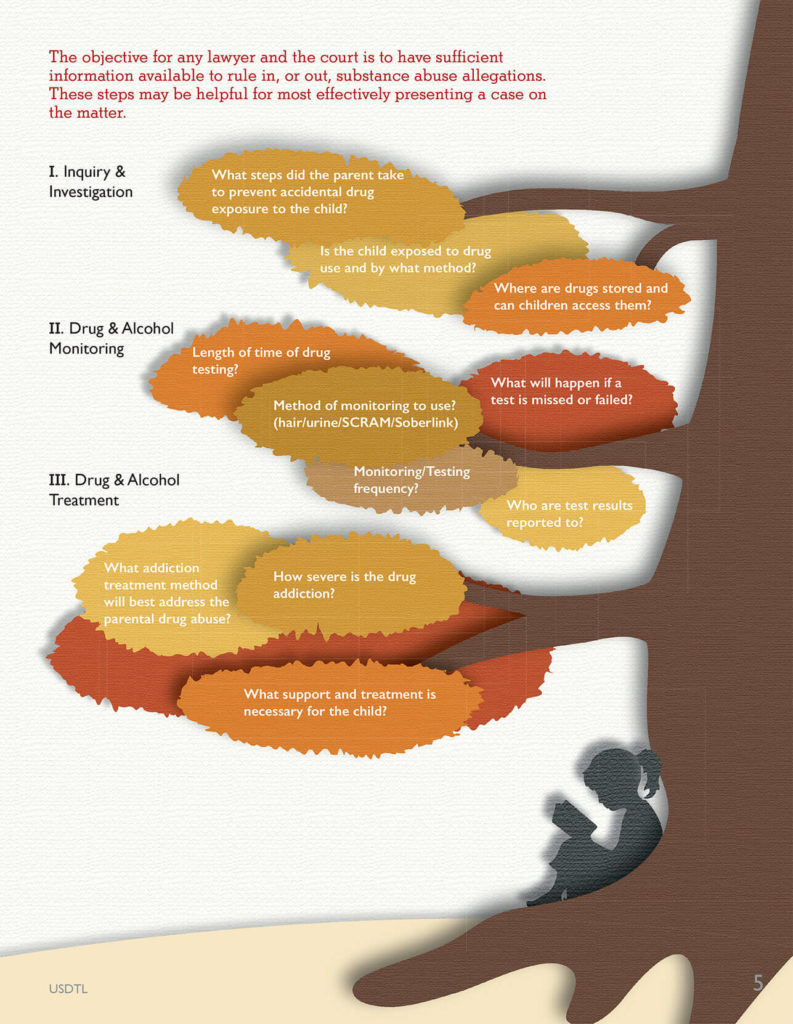
The objective for any lawyer and the court is to have sufficient information available to rule in, or out, the substance abuse allegations. This information may be presented via admissible evidence, witness testimony, and/or expert testimony. The following pointers may be helpful to legal professionals so that they are able to most effectively present a case on this matter.
Step 1 – Inquiry & Investigation
One of the first steps in evaluating a substance abuse allegation is to ask research informed questions so that the most relevant data can be gathered. Questions should be focused on potential exposure of the children to parental drug possession or use. For example, relevant questions may include:
- Where does the defendant allegedly store the drugs?
- Does the child have easy access to these storage containers and locations?
- Is the child typically present when the drugs are used?
- In what ways may the child have been exposed?
- What steps, if any, did the parent take to protect the child from accidental exposure?
Step 2 – Drug & Alcohol Monitoring
If a parent tests positive on an alcohol or drug test, this may result in a motion, agreement, or court order for ongoing monitoring. However, many questions then arise. For example, how long should the monitoring extend? Should it
include both alcohol and drugs? What type of drug monitoring method should be used (urine/hair/SCRAM/Soberlink, etc.)?
Celebrating 10 Years of Forensic Toxicology Innovation Using LCMSMS Technology
By Joseph Jones, MS, NRCC-FTC
Ten years ago, USDTL, Inc. was a much different laboratory than it is today. Back then, we still had yet to develop fingernail, umbilical cord, or dried blood spot phosphatidylethanol (PEth) testing. We weren’t even testing ethyl glucuronide (EtG) in urine or hair, our most common form of alcohol testing today. But, as it turns out, ten years ago was right at the turning point for us, that moment of tremendous innovation and acceleration that has pushed us to the forefront of forensic toxicology we are at now. One of our biggest leaps forward at that time was adopting liquid chromatography (LC) technology into our methodology and moving from a solely gas chromatography (GC) focused laboratory to an integrated GC/LC facility. We’ve never looked back.
Our first LC instrument was generically dubbed machine Number 7, and it was a gamble for us. We had very little experience with LC methodologies, and we were not actively looking to adopt that technology at that time. In 2005 we were approached by the analytical technology company AB Sciex, who were looking to increase their competitive share of the forensic testing field, specifically with their liquid chromatography tandem mass spectrometry (LCMSMS) instruments. They made us an offer we couldn’t refuse – a new LCMSMS instrument in our lab, assistance in developing a new EtG/EtS urine assay, and six months to develop our market. After six months, they would let us decide whether or not we wanted to buy the instrument, or take a pass and send it back. What growing laboratory would ever say no to that?
As soon as assay development was complete, we starting receiving requests for urine EtG/EtS testing from all over the country. Major labs such as LabCorp and Witham labs relied on us to do all of their EtG/EtS testing. Six months came and went, and not only could we afford to keep Number 7, but we had built enough business to occupy two machines, and Number 9 was purchased as well. Number 9 passed on to new owners just a few years ago, but good ol’ Number 7 is still chugging away in our lab, having processed well over 100,000 samples in those 10 years. It’s a well-loved work horse to this day.
That offer from AB Sciex came out of the blue without warning, and for us, it was a major shake-up. We could have said “no thank you,” but we didn’t. Even with the generous offer made by AB Sciex, this course of action was a big risk for us. We took a chance on an opportunity to extend our innovation, as well as build a fantastic partnership that has endured these ten years. The net result was a powerful expansion of our instrumental capabilities that has allowed us to bring major innovations to the forensic testing world, such as umbilical cord testing, dramatically improved sensitivity in cannabinoid testing, PEth testing in dried blood spots, and more. Incorporating LCMSMS technology into our methodologies has allowed us to leverage our expertise to create what was previously not possible. It is a key factor in making USDTL first in newborn toxicology and without question the best hair and fingernail testing lab in the U.S.
Ten years on, we raise our glass to good ol’ Number 7, to the past 10 years of pushing the boundaries of forensic toxicology, and to another 10 years and beyond of making a difference in the world around us.
- Hair, Nail, and Umbilical Cord Testing for Phenibut, Medetomidine, and Tianeptine
- Umbilical Cord Tissue Testing for SSRIs
- A Comparison of Turnaround-Times for Two Popular Specimen Types Used for Newborn Toxicology: Meconium and Umbilical Cord Tissue
- Using Umbilical Cord Tissue to Identify Prenatal Ethanol Exposure and Co-exposure to Other Commonly Misused Substances
- Toxicology as a Diagnostic Tool to Identify the Misuse of Drugs in the Perinatal Period
- Specimen Delay
- Drug Classes and Neurotransmitters: Amphetamine, Cocaine, and Hallucinogens
- Environmental Exposure Testing for Delta-8 THC, Delta-9 THC, Delta-10 THC, and CBD
- February 2025 (1)
- October 2024 (5)
- March 2024 (1)
- February 2024 (1)
- January 2024 (3)
- December 2023 (1)