Blog

Congratulations to Michelle Pilkington for joining the Board of Directors for the Chicago Chapter of the Clinical Laboratory Management Association. CLMA is a community that brings together clinical laboratory professionals from laboratories of all sizes. Clinical laboratory managers and leaders, clinical technicians, consultants, marketers and military staff can connect and share their collective knowledge. To learn more click here. Michelle said “Having a seat at the table, representing USDTL, gives us an opportunity to be face to face with some of our regional clients and make a difference.”

At the 2019 annual business meeting of the Society of Forensic Toxicologists (SOFT) on October 17, 2019, Andre Sukta was elected by the membership to be on the Board of Directors. The Board of Directors are tasked with representing the members at large and providing mission-based leadership, strategic governance and leadership continuity. The mission of SOFT is to be an organization composed of practicing forensic toxicologists and those interested in the discipline for the purpose of promoting and developing forensic toxicology. “It is an honor that my professional colleges have entrusted me with this responsibility and I look forward to continuing and honoring the legacy of this organization” Andre said. Please join USDTL in congratulating Andre for such an incredible achievement!

There are many variables regarding the analyses of substance abuse testing. Clients will often ask about specifics pertaining to the determination of time, dose and frequency when detecting substance(s) of abuse.
When testing a reservoir matrix- a material or substance which can accumulate and retain drug and alcohol biomarkers (eg., urine, blood, hair, nail, umbilical cord, or meconium, etc.), the reported quantitation of a drug or its metabolite cannot be used to determine when/if a specific substance was used, how much of a substance was used or how often a substance was used. Test results show only if a substance was detected or not detected.
A specimen’s window of detection provides an estimated timeframe for detecting substance(s) of abuse. Based on extensive research studies, the generally accepted windows of detection for specimens used in our testing are as follows:
- Scalp Hair- Up to approximately 3 months prior to collection.
- Fingernail- Up to approximately 3-6 months prior to collection.
- Umbilical Cord- Up to approximately 20 weeks prior to birth.
- Meconium- Up to approximately 20 weeks prior to birth.
- Urine- Up to approximately 2-3 days prior to collection.
- Blood (PEth)-May be up to approximately 2-4 weeks prior to collection.
It is important to know that the interpretation of drug testing results may be determined by a Medical Review Officer (MRO). A Medical Review Officer is a licensed physician (MD or DO) who has knowledge of substance abuse disorders and has the appropriate medical training to interpret and evaluate an individual’s positive test result together with his or her medical history and any other relevant biomedical information.1This is an incredibly important aspect of drug testing. A laboratory can detect substances, but an MRO may be used to interpret what that detection means.
1. Journal of Occupational and Environmental Medicine: (January 2003-Volume 45-Issue 1-p 102-103) Qualifications of Medical Review Officers (MRO’s) in Regulated and Nonregulated Drug Testing. Departments: ACOEM Consensus Opinion Statement

By Adobe Stock©
According to the Centers for Disease Control and Prevention (CDC), fentanyl-related overdose deaths in the United States have increased by more than 1,000 percent from 2011 through 2016.1 The increased availability of illicitly manufactured fentanyl has contributed to the prevalence of neonatal abstinence syndrome (NAS) or neonatal opioid withdrawal syndrome (NOWS) throughout the United States. There was a greater than five-fold increase in the proportion of babies born with NAS from 2004 to 2014, when an estimated 32,000 infants were born with NAS/NOWS —equivalent to one baby suffering from opioid withdrawal born approximately every 15 minutes.2
In response to an ongoing opioid epidemic, medical professionals and advocates are invested in providing education, resources, testing, and preventative care in efforts to combat one of the most powerful opioids in the world —Fentanyl. This synthetic, opioid is extremely addictive and when used while pregnant can cause devastating outcomes to the fetus including neural tube defects, congenital heart defects, gastroschisis, stillbirth, and pre-term delivery.3
Newborns are often diagnosed with NAS/NOWS as a direct result of a sudden interruption of fetal exposure to prescription and illicit substances that were used or abused by the mother. Diagnosing an infant with NAS/NOWS is often assessed by identifying the following symptoms: tremors, jitteriness, irritability, excessive crying, and diarrhea. These indicators have been determined in the medical field as the standards for identifying a compromised central nervous system. Prenatal use & abuse of fentanyl can increase an infant’s risk for developing NAS/NOWS.
What Makes Fentanyl So Dangerous?
According to the United States Drug Enforcement Administration (DEA), fentanyl is approximately 100 times more potent than morphine and 50 times more potent than heroin.4 Its initial development was intended as a licit intravenous anesthetic; however, it has now become a public health threat as pharmaceutical products are subjected to theft, fraudulent prescriptions and illicit or less regulated distribution and manufacturing. The drug is often abused by injecting, snorting / sniffing, oral tablets/pills or removing the gel on fentanyl patches and then injecting or ingesting. The popularity of fentanyl within drug addicted communities derive from the addictive effects the drug produces —relaxation, euphoria, pain relief, and sedation. However, abused fentanyl also produces fatal side effects including: confusion, dizziness, nausea, vomiting, urinary retention, pupillary constriction, and respiratory depression.
Fentanyl’s Long-Term Effects on Fetus
Prenatal substance abuse can lead to long-term, irreversible damage to a developing fetus. In relation to fentanyl, these effects can consist of the following when associated with NAS/NOWS:5
- Cognitive and motor development deficiencies
- Infections
- Vision complications
- Sudden Infant Death Syndrome (SIDS)
- Susceptible to future substance abuse
Fentanyl and Toxicology Confirmation
According to the American Academy of Pediatrics, NAS/NOWS is a clinical diagnosis, however toxicological confirmation is necessary to identify the exact type of substance that the mother was using or abusing and to confirm or rule out the use of other licit or illicit substances during pregnancy.6
Due to the recent increase of cases regarding pregnant women and fentanyl exposure, it is critical to utilize testing that can help detect the latest drugs of abuse. Through internal research and strategic analysis, our laboratory is combating the growing epidemic of fentanyl use among pregnant women and those of childbearing age, with the development of testing for fentanyl in both umbilical cord tissue and meconium. As the first and only laboratory to offer fentanyl testing utilizing both advanced newborn specimens, our partnerships are provided with the opportunity to proactively and effectively address the alarming rates of prenatal fentanyl use. Both meconium and umbilical cord tissue belong to the baby, therefore maternal consent is not needed to proceed in testing.
Umbilical Cord Tissue
The umbilical cord tissue is available immediately for 100 percent of births and requires only 1 collection by 1 collector. This specimen’s look back provides detection up to approximately 20 weeks prior to birth, the most advanced newborn specimen on the market.
Meconium
Meconium has been recognized for decades as the “gold standard” for the detection of substances. It is the first stool of an infant produced in utero, consisting of epithelial cells, bile, mucous, and is odorless with a very dark, tar-like appearance. Meconium is uniquely developed during gestation with exclusive capabilities of preserving substances exposed prenatally up to approximately 20 weeks prior to birth. The average start of a meconium passage after birth occurs within 24-48 hrs., in most newborns it is generally passed in the first day or so of life.
Turnaround Time
Our methodology and advanced instrumentation contribute to our laboratory’s efficient turnaround time. Generally, the standard turnaround time for reporting negative screening test results is the next business day, with an additional 1-2 business days for specimens that require confirmatory testing. Turnaround time begins from receipt of the valid specimen–accompanied by a properly documented valid order– into the laboratory. Some tests require additional time to process and will fall outside the standard turnaround time window.
As one of the only laboratories in the nation focusing exclusively on substance abuse testing, we are consistently adapting our services to meet the needs of our clients and communities. The validity of newborn toxicology results has never been more imperative. Through our partnership and services, we can customize a flexible comprehensive drug testing program based on your population health needs. Today’s substance abuse landscape is drastically different than it used to be-collaboration is vital in supporting our mission of protecting and enriching lives.
References
- Spencer, M.P.H., M., Warner, Ph.D, M., Bastian, B.S., B., Trinidad, M.P.H., M.S., J. and Hedegaard, M.D., M.S.P.H., H. (2019). “National Vital Statistics Reports.” [online] Cdc.gov. Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_03-508.pdf [Accessed 17 Sep. 2019].
- Drugabuse.gov. (2019). “Dramatic Increases in Maternal Opioid Use and Neonatal Abstinence Syndrome.” [online] Available at: https://www.drugabuse.gov/related-topics/trends-statistics/infographics/dramatic-increases-in-maternal-opioid-use-neonatal-abstinence-syndrome [Accessed 17 Sep. 2019].
- Center for Disease Control and Prevention, U. (n.d.). “Pregnancy and Opioid Pain Medications.” Retrieved from https://www.cdc.gov/drugoverdose/pdf/pregnancy_opioid_pain_factsheet-a.pdf.
- Department of Education, U. (n.d.). “Drugs of Abuse Guide” (2017)(pp. 40-41) (United States).
- “Long-Term Outcomes of Infants With Neonatal Abstinence Syndrome.” (n.d.). Retrieved from https://www.seattlechildrens.org/healthcare-professionals/education/continuing-medical-nursing-education/neonatal-nursing-education-briefs/long-term-outcomes-of-infants-with-nas/
- Kocherlakota, P. (2014, August 01). “Neonatal Abstinence Syndrome.” Retrieved from http://pediatrics.aappublications.org/content/134/2/e547
By Kelly Hack, Content Writer
According to the United States Drug Enforcement Agency (DEA), methamphetamine seizures have proliferated over the last eight years, increasing from 8,900 pounds in 2010 to nearly 82,000 pounds in 2018.1 This stimulant’s aggressive nature is spreading its toxicity predominantly in rural areas including Oklahoma, Virginia, and Kentucky. The power of methamphetamine has captured countless lives and, in the U.S. alone, the number of overdose deaths increased 3.6-fold from 2011 to 2016.2
Methamphetamine, once used to keep troops awake during World War II, quickly took a turn for the worse in Central Europe when Japanese chemist, Akira Ogata discovered the ease in manufacturing the drug simply by using over-the-counter cough medication (pseudoephedrine) and household cleaning products.2 Methamphetamine, a classified stimulant substance is identified as a white, bitter-tasting powder or pill. Crystal methamphetamine, an additional form of the drug is a psychostimulant that resembles glass fragments or shiny rocks, hence its street names crystal or ice.3

Methamphetamine can be abused in several forms including:
- Inhaling/Smoking
- Swallowing
- Snorting
- Injecting3
The substance produces an extreme amount of dopamine (3x more than cocaine), triggering the reward receptors in the brain.3 Within seconds of using, an adrenaline-like rush begins, which is accompanied by a euphoric high that can last for hours, and ultimately followed by an overwhelming, crippling comedown. Crystal meth activates the neurotransmitters: serotonin and norepinephrine, which can elevate blood pressure and heartbeat, causing stimulation, loss of appetite, and irritability/aggressiveness.2 The false sense of exhilaration this drug produces leads to its repeated use. The short-term effects of this drug are often what entice a user to use repeatedly. Chasing this drug’s original rush is what provokes the insidious cycle of methamphetamine addiction.

Long-Term Effects
- Higher susceptibility to contracting HIV/AIDS, Hepatitis B and C due to altered judgement leading to risky sexual behaviors.
- Extreme weight loss
- Severe dental complications
- Skin eruptions
- Anxiety
- Confusion
- Insomnia/disrupted sleep
- Violent behavior
- Mental illness-paranoia/hallucinations3
Combating Methamphetamine On A National Level
In efforts to combat the plague of methamphetamine and to put a halt to at-home chemists, in 2006 The Combat Methamphetamine Epidemic Act was enacted, limiting over-the-counter access to cold medications containing essential ingredients to manufacture the drug. This act significantly reduced domestic meth labs, where amateur chemists produced meth by using “shake and bake” techniques consisting of cold medicine, toxic chemicals, and an empty two-liter bottle. As domestic methamphetamine labs were shut down one by one, aggressive drug cartels began to dominate the black market. Drug gangs began to navigate across the U.S.-Mexico border using drones, fuel tanks, batteries, and juice bottles to smuggle drugs.2 Currently, most of the methamphetamine found in the United States derive from clandestine “superlabs” in Mexico. These labs produce hundreds of pounds of methamphetamine daily.3
The Global Impact of Methamphetamine
The United States is not alone in its effort to seize criminal networks contributing to the availability of methamphetamine among communities. A dozen countries including China and Germany are reporting that methamphetamine is their primary drug of concern. Since 2008, the global market has expanded more than sixfold. Global crime rings and traffickers have developed encrypted phones and darknet communication to namelessly purchase drugs, along with adjusting drug formulas to maneuver around the DEA and other associated agencies.3

Medical Impacts of Methamphetamine
The influx of this drug’s attainability has increased occurrences of violence, arrests, ambulance calls, hospital admissions, and psychiatric services–creating a heavy burden to the lives of many. In the U.S., meth-related hospital costs reached $2.17 billion in 2015.3 In 2017,16.6% of women with primary and secondary syphilis (P&S Syphilis) used methamphetamine. Primary syphilis is the beginning stage of the sexually transmitted disease (STD) and can be identified by single or multiple sores lasting 3 to 6 weeks. The secondary stage of syphilis begins to expose more severe symptoms such as mucus membrane lesions and swollen lymph nodes.4 These findings support that a large percentage of heterosexual syphilis transmission is occurring at an increased rate with those that abuse methamphetamine.5 Among pregnant women, admissions for the treatment of methamphetamine abuse increased from 8% in 1994 to 24% in 2006. Case reports and retrospective analysis have indicated that maternal methamphetamine use may be attributed to defects of the fetal central nervous system, cardiovascular system, gastrointestinal system, as well as oral cleft and limb defects.6
Due to the severity of methamphetamine and the adverse effects it creates with its use, incorporating advanced testing panels into your organization’s drug testing efforts can be an effective approach to detecting potential use & abuse of this dangerous substance. Our laboratory offers methamphetamine testing for adult, child, and newborns, utilizing specimens such as fingernail, hair, meconium, umbilical cord tissue, and urine. By providing the most comprehensive panels within the drug testing market, we help organizations address the prevalence of substance abuse that affects so many of us today.
Kelly Hack, Content Writer for USDTL holds a Master’s of Science in Journalism, along with a versatile professional portfolio including investigative, educational, feature, and profile writing. Hack currently strives to capitalize her knowledge-base in efforts to provide readers with information that is accurate, concise, and pertinent.
References:
1. “DEA releases 2018 National Drug Threat Assessment.” (n.d.). Retrieved from https://www.dea.gov/press-releases/2018/11/02/dea-releases-2018-national-drug-threat-assessment-0
2. (n.d.). Retrieved from https://www.bloomberg.com/news/articles/2019-04-03/cheap-nasty-near-you-how-crystal-meth-is-spreading-quicktake
3. National Institute on Drug Abuse. (n.d.). “cccc.” Retrieved from https://www.drugabuse.gov/publications/drugfacts/methamphetamine
4. STD Facts – Syphilis. (n.d.). Retrieved from https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm
5. “Increased Methamphetamine, Injection Drug, and Heroin Use Among Women and Heterosexual Men with Primary and Secondary Syphilis” – United States, 2013–2017 | MMWR. (n.d.). Retrieved from https://www.cdc.gov/mmwr/volumes/68/wr/mm6806a4.htm
6. Women’s Health Care Physicians. (n.d.). Retrieved from https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Methamphetamine-Abuse-in-Women-of-Reproductive-Age
by: Kelly Hack
The National Drug Early Warning System (NDEWS) funded at the Center for Substance Abuse Research by the National Institute on Drug Abuse (NIDA) presents a compelling methodology of leveraging an innovative overdose detection mapping application program (ODMAP) with collective partnerships to address the overdose epidemic of opioids.
In efforts to bridge the gap of public health and public safety, ODMAP provides real-time suspected overdose surveillance data across jurisdictions throughout the nation. The development of this online mapping portal provides first responders, hospitals, and other law enforcement agencies the ability to communicate and record vital information utilizing a time-sensitive approach.
Program Accessibility
Level 1-Data Collection and Agency Administration Interface:
The system was designed to minimize the effort and time required by a first responder to enter data including fatal or non-fatal overdoses and the extent to which naloxone or another reversal drug was administered.
Level-1-API Data Collection:
The Application Programming Interface (API) is an extended option for Level 1 users, providing an effective method for stakeholder agencies to contribute data without creating additional (manual) reporting or processes. The API integration connects with agency or state’s Record Management Software (RMS) to ODMAP with an automated assimilation of the two systems.
Level 2-National Map:
In efforts to monitor and measure the performance of criminal justice and public health functionality, the ODMAP dashboard is an available tool for decision-makers to view and analyze controlled unclassified information (CUI) at a nation level. This tool is exclusive to government agencies (state, local, federal, or tribal) serving the interests of public safety and health.
Statewide Implementation
Since ODMAP’s inception, the program has gained an increased popularity throughout the nation. The Illinois Law Enforcement Alarm System (ILEAS) and the Illinois Department of Public Health (IDPH) have developed a grant titled, “Empowering and Equipping Law Enforcement and Communities in Rural Illinois to Reduce Opioid Overdose,” requiring the onboarding of ODMAP.
Spike Alerts
In order to support the needs of communities, health analysts developed ODMAP’s spike response framework, which notify agencies by email, if the total overdoses in an area exceeds a pre-determined threshold within a 24-hour period. Spike alerts can be established for an agency’s own county or surrounding counties as an early warning feature.
An Innovative Initiative
As a laboratory who is invested in protecting and enriching lives, we support innovative developments that present effective advancements for addressing a drug epidemic that nationally has claimed over 72,000 overdose deaths. Mobilizing a cohesive and collaborative response to a complex drug crisis is imperative within our communities.
For more information regarding ODMAP, visit www.odmap.org.
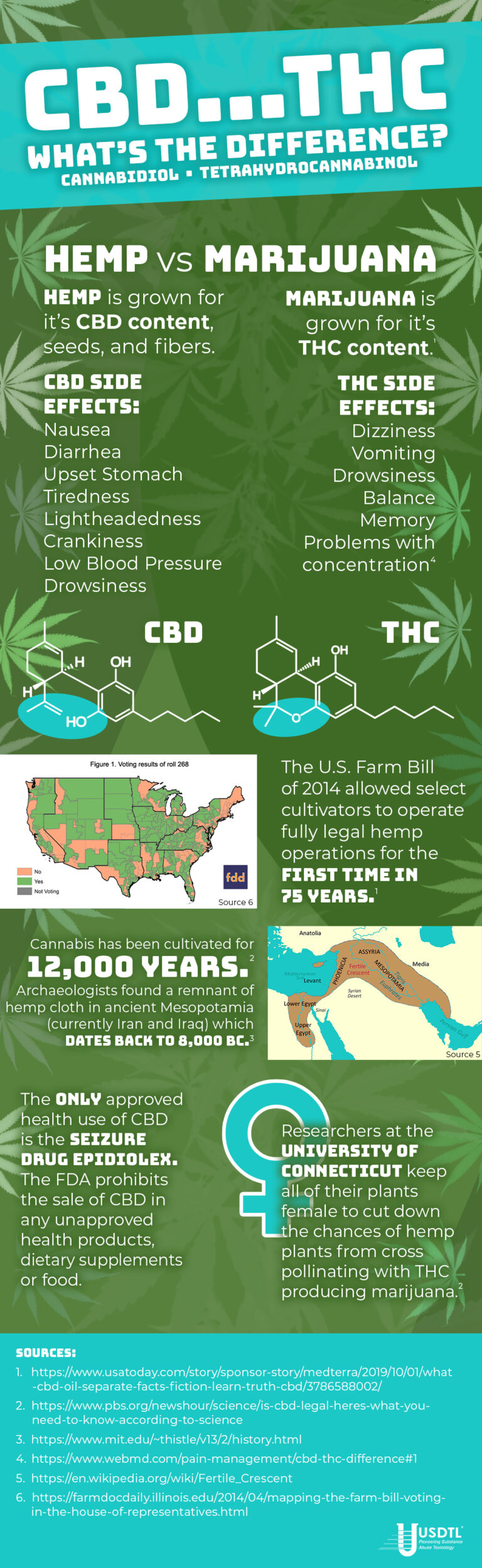
An alarming rise in benzodiazepine-related morbidity and mortality is a growing concern in the U.S., research has concluded that 919 benzodiazepine ambulatory visits occurred in 2003 and increased drastically to 1672 in 2015.1 The reported ambulatory visits have resulted in a 127 percent increase in benzodiazepine-related deaths or injuries. Amid the opioid crisis, benzodiazepine use/abuse is significantly growing with more than 30 percent of overdoses involving opioids also involve benzodiazepines.2
To provide a better understanding of how powerful benzodiazepines are, the medical realm has defined the substance as a tranquilizer that acts on the central nervous system producing sedation and muscle relaxation. The following benzodiazepines are classified by their length of effect:
- Ultra Short Acting-Midazolam (Versed®) and Triazolam (Halcion®)
- Short Acting- Alprazolam (Xanax®) and Lorazepam (Ativan®)
- Long Acting-Chlordiazepoxide (Librium®) and Diazepam (Valium®)3
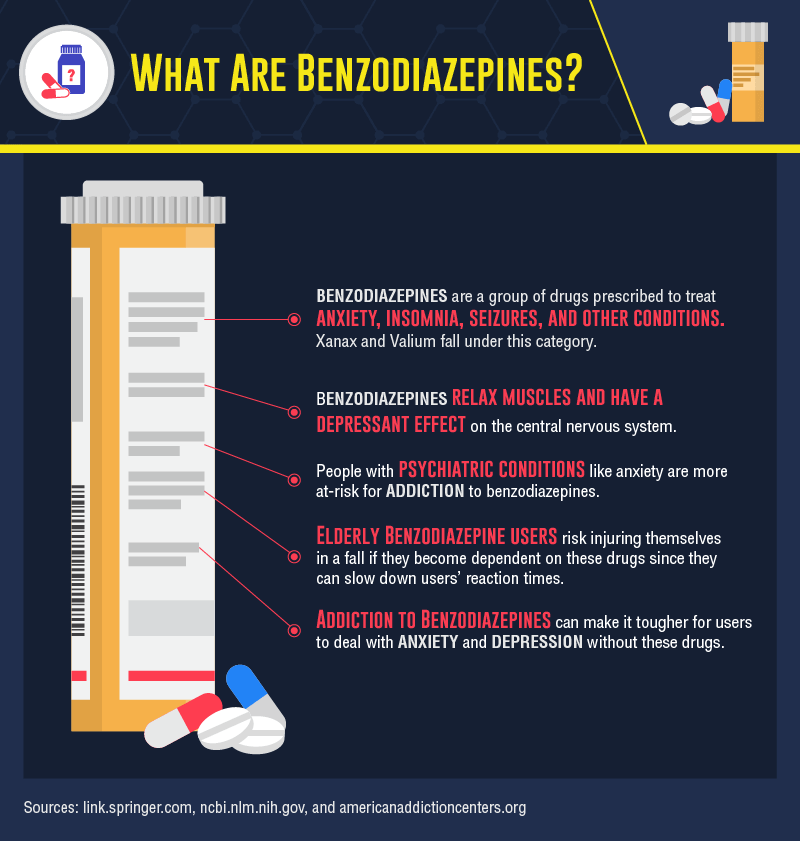
According to a 2018 study, 30 million Americans used benzodiazepines in the past year and of those more than 5 million misused them for purposes of a sleep aid or to get high.4 Benzodiazepines can lead to physical and psychological dependence. In fact, high doses of benzodiazepines can create signs and symptoms of acute toxicity or overdose including drowsiness, confusion, dizziness, blurred vision, weakness, slurred speech, difficulty breathing and even coma.3
Despite the risks associated with benzodiazepines, research and statistics are finding that there has been a spike in prescribing in lieu of the opioid crisis. A study from 2003-2015 indicated a substantial increase of primary care physicians (PCP’s) who are issuing prescriptions for benzodiazepines-3.6 percent to 7.5 percent.1 Primary care physicians defined by the National Ambulatory Medical Care Survey (NAMCS) includes: family medicine, internal medicine, geriatric medicine and obstetrics and gynecology. The increased number of benzodiazepine visits suggests there is a growing number of patients being prescribed this drug, along with prescriptions written for long-term use.
In 2015, 23 percent of people who died of an opioid overdose also tested positive for benzodiazepines.2 In a 2016 study, researchers noted that when opioids and benzodiazepines are used simultaneously, a 570 percent increase in substance abuse treatment admissions occurred.4 Co-prescribing, which is defined as prescribing two or more drugs to the same patient is an apparent, yet overlooked contributing factor to the drug epidemic we are facing today.
In 2015, benzodiazepines were co-prescribed with an opioid in 19.2 percent of visits, opioids were co-prescribed with a benzodiazepine in 26.4 percent of visits.1 As opioids lose favor among prescribers, it is imperative to be aware of the risks that are associated with benzodiazepines, especially when used in combination with an opioid. It is strongly advised that clinicians avoid prescribing benzodiazepines concurrently with opioids.
In 2016, the FDA required benzodiazepines to be “black box” labeled in efforts to warn patients about the drug’s side effects and the heightened risks when taken with opioids. As a Schedule III drug, benzodiazepines have an increased probability for dependency. Physicians are advised to prescribe with caution, to fully inform their patients of the risks involved with benzodiazepines and the threat of fatality when combined with an opioid.
Utilizing advanced drug testing, specifically for benzodiazepines can be a proactive approach in identifying potential at-risk behavior and preventing fatal outcomes. Advanced drug testing uses different specimen types to detect substances of abuse at different times. Depending on the specimen’s window of detection, short-term and long-term use can be identified as the following:
Short-Term:
- Urine- 2-3 days
- Oral Fluid-1-2 days
- Blood-1-2 days
Long-Term:
- Hair- 3 months
- Fingernail-3-6 months
Utilizing an accredited laboratory that offers extensive panels to test for drugs of abuse is imperative in counteracting the impending drug crisis of benzodiazepines.
Benzodiazepines in Hair Benzodiazepines in Nail
Benzodiazepines in ChildGuard Benzodiazepines in Urine
References:
- Agarwal, S. D. (2019, January 25). Patterns in Outpatient Benzodiazepine Prescribing in the United States. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2722576
- National Institute on Drug Abuse. (2018, March 15). Benzodiazepines and Opioids. Retrieved from https://www.drugabuse.gov/drugs-abuse/opioids/benzodiazepines-opioids
- Benzodiazepine Abuse. (n.d.). Retrieved from https://www.webmd.com/mental-health/addiction/benzodiazepine-abuse
- Smith, M. (2019, February 06). After Opioids, Benzodiazepine Use Raises Concern. Retrieved from https://nida.nih.gov/research-topics/opioids/benzodiazepines-opioids
- Umbilical Cord Tissue Testing for SSRIs
- A Comparison of Turnaround-Times for Two Popular Specimen Types Used for Newborn Toxicology: Meconium and Umbilical Cord Tissue
- Using Umbilical Cord Tissue to Identify Prenatal Ethanol Exposure and Co-exposure to Other Commonly Misused Substances
- Toxicology as a Diagnostic Tool to Identify the Misuse of Drugs in the Perinatal Period
- Specimen Delay
- Drug Classes and Neurotransmitters: Amphetamine, Cocaine, and Hallucinogens
- Environmental Exposure Testing for Delta-8 THC, Delta-9 THC, Delta-10 THC, and CBD
- Bromazolam and Synthetic Benzodiazepines
- October 2024 (5)
- March 2024 (1)
- February 2024 (1)
- January 2024 (3)
- December 2023 (1)
- November 2023 (1)