Blog

What is Buprenorphine?
Buprenorphine is a derivative of thebaine, an extract of opium. Buprenorphine is an opioid partial agonist, meaning it can activate the opioid receptors in the brain, but to a lesser degree than opioids such as heroin.
Partial agonist drugs like buprenorphine, butorphanol, and tramadol can be helpful for treating pain and can assist in treating opioid use disorder, as they can help minimize withdrawal symptoms. Buprenorphine has a ceiling effect, causing a plateau in the sedative effects, which helps protect the individual from negative respiratory and/or cardiovascular effects when taken as prescribed.
Buprenorphine has been used internationally for several years to assist people suffering from opioid dependency. Subutex, which is pure buprenorphine, is designed to be used in the initial stages of addiction treatment.1
Buprenorphine Misuse and Diversion
As the opioid crisis started growing, treatment drugs such as buprenorphine were being looked at for misuse and diversion. In 2014, the Food and Drug Administration required new safety labeling on prescribed opioids, indicating they are a Schedule III drug and warning of “risks of addiction, abuse, and misuse, which can lead to overdose and death.”3
According to the National Drug Intelligence Center, Suboxone (buprenorphine and naloxone)–because of its ceiling effect and ability to precipitate withdrawal systems if taken in high doses– is more susceptible to misuse by individuals who are addicted to low doses of opioids or individuals in the early stages of opioid addiction.1
Misuse may include mixing buprenorphine with other drugs, such as heroin or methamphetamine, for a more intense high. Buprenorphine misuse is extremely dangerous even though it is used in clinical settings. In those settings, buprenorphine is administered in small, specifically curated doses based on the patient’s substance use history.
Diversion of buprenorphine, or nonmedical use by people it is not prescribed for, is another potential risk for consideration. According to the Center for Disease Control’s (CDC) 2022 Clinical Practice guidelines for prescribing opioids, toxicology tests can assist clinicians in identifying when patients are not taking opioids prescribed for them, which may indicate diversion or other clinically important issues such as difficulties with adverse effects.3 Advanced specimen drug testing may be the link to identifying the misuse or diversion of buprenorphine.
USDTL Advanced Specimen Testing
As an innovative leader offering alcohol and other drug testing, we understand the importance of being able to test for drugs of concern when it is most feasible for your organization. We offer buprenorphine testing, along with testing for many other drugs of concern, in urine, nail, and hair specimens. Contact us at adultandchild@usdtl.com with any questions.
References:
- https://www.justice.gov/archive/ndic/pubs10/10123/index.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3154701/
- https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm

By Canva© Studio
Xylazine is a sedative which causes analgesic and muscle-relaxing properties and is approved for veterinary medicine. Xylazine was first produced in 1962 by the Bayer company1. It has been studied for human use, but clinical trials had to be terminated due to severe adverse side effects, including central nervous system (CNS) depression1. Xylazine is not approved for human consumption, but it has been found as an adulterant being added to drugs, and it has been used in drug facilitated crimes to induce sleep. According to the DEA, there were 149 reported cases from federal and state laboratories involving xylazine in 2015, but that number jumped to 8,938 in 20211.

By Canva© Studio
Some individuals exposed to xylazine may not be aware of its presence. Xylazine has been found as an adulterant in white powder drugs. Primarily xylazine has been detected in heroin and fentanyl supply, though it has also been discovered in some stimulant supply such as methamphetamine and cocaine2. Other users actively seek out and use xylazine along with speedball, the street name for a mixture of heroin and cocaine, to mitigate some of xylazine’s negative effects. Xylazine containing products can be marketed on the street as tranq, sleep-cut, Philly-dope, or zombie drug.
Negative side effects of xylazine include CNS and respiratory depression, hypotension, hypothermia, high blood glucose levels, miosis, hypotension, and necrotic skin ulcerations that can lead to amputation if not treated. Additionally, because xylazine is not an opioid, naloxone is ineffective in the event of an overdose. The FDA issued a safety alert warning in November 2022 about the severe risks associated with the drug3.
Xylazine is not currently scheduled, though legislation was proposed in March 2023 to make xylazine a Schedule III Substance4. Congress has considered scheduling the substance prior to this legislation, but scheduling the drug would significantly impede the veterinary use of the medication5. Currently, the FDA is working to more strictly regulate the importation of xylazine and verify the legitimate veterinary supply6.
- https://www.deadiversion.usdoj.gov/drug_chem_info/Xylazine.pdf
- https://www.fda.gov/media/162981/download
- https://www.empr.com/home/news/safety-alerts-and-recalls/fda-restricts-unlawful-import-of-xylazine-containing-products/#:~:text=In%20November%202022%2C%20the%20FDA,and%20high%20blood%20glucose%20levels.
- https://abc7chicago.com/xylazine-effects-in-humans-congress-controlled-substance/13043734/
- https://www.avma.org/blog/congressional-offices-consider-making-xylazine-controlled-substance
- https://www.fda.gov/news-events/press-announcements/fda-takes-action-restrict-unlawful-import-xylazine
Sign up here to learn more and receive our newsletter on the latest updates with USDTL.

What is Ketamine?
Ketamine (ketamine hydrochloride) is a dissociative anesthetic with some hallucinogenic effects, meaning it distorts perceptions of sight and sound and makes the user feel disconnected from their environment and any pain.1 It has one-tenth the potency of PCP, and its original use is as an injectable, short-acting anesthetic for use in humans and animals.5 Ketamine can induce a state of sedation (feeling calm and relaxed), immobility, relief from pain, and amnesia (no memory of events while under the influence of the drug).1 It can be used for the induction (the transition from an awake to an anaesthe-tized state) of general anesthesia as a pre-anesthetic to other general anesthetic agents.2
Potential Therapeutic Use
Studies from Yale research labs showed that ketamine triggers “glutamate production,” which can prompt the brain to form new neural connections. This makes the brain more adaptable and able to create new pathways, giving patients the opportunity to “develop more positive thoughts and behaviors.” This was an effect that had not been seen before, even with traditional antidepressants.4 For the last two decades, researchers at Yale have led ketamine research by experimenting with using small doses of ketamine delivered intravenously in controlled clinical settings for patients with severe depression who have not improved with standard antidepressant treatments. In several studies, more than half of participants (who felt other antidepressant medications were ineffective) showed a significant decrease in depression symptoms after just 24 hours. The study states that ketamine “needs to be part of a more comprehensive treatment plan.”4 Studies are continuing to explore the possibilities of ketamine in therapeutic settings. It is not unlikely to assume that as ketamine gets clinically used, it will unfortunately also be under threat of being abused or misused.
Ketamine Misuse
Much like its intended use, ketamine can be misused recreationally for its ability to produce dissociative sensations and hallucinations. In 2022, the American Addiction Centers reported that nonmedical misuse is relatively low, with 0.7% of the U.S. population using it illegally.6
Since ketamine can be used in powdered form, it has been known to be snorted as a “party drug” at festivals or rave events.3 The street name for ketamine is “K” or “Special K.”
Ketamine has also been used to facilitate sexual assault because of its hallucinogenic effects known to make the user feel disconnected from their surroundings. A number of individuals have abused this drug or have been instrumental in others using this drug as a “date-rape” drug.1
Recreational use of ketamine can result in a number of internal complications including:
- gastrointestinal issues;
- depression;
- respiratory problems and;
- amnesia
Serious debilitating urinary tract symptoms are also seen frequently in those individuals who abuse ketamine.3 A study on ketamine in the National Institutes of Health predicts that ketamine toxicity and addiction “pose significant risks to a small segment of the population, and given increasing utilization, the prevalence of these phenomena is expected to increase.5” As ketamine use increases both recreationally and clinically, it will continue to be a substance worth testing for.
USDTL Testing
As an innovative leader offering alcohol and other drug testing, we understand the importance of being able to test when it is most feasible for your organization. We offer extended panel testing for ketamine in alternative specimens including hair, nail, and urine.
References:
- 3: https://clinmedjournals.org/articles/ijda/international-journal-of-depression-and-anxiety-ijda-1-006.php?jid=ijda
- 4: https://www.yalemedicine.org/news/ketamine-depression
- 5: https://www.ncbi.nlm.nih.gov/books/NBK541087/
- 6: https://americanaddictioncenters.org/ketamine-abuse

ToxTime: Choose the Best Test – An Overview of Advanced Alcohol & Other Drug Testing Options
Please join us for ToxTime with Guida Brown, Guided by Guida, discussion over detection windows for a variety of drug and alcohol tests.
Description:
Choosing the best test is determined by what information is sought. Testing of urine, blood, hair, or nails, among other substances, each serves a purpose, but the right test is needed for the results to be useful to anyone. During this free ToxTime presentation, Guida Brown of Guided by Guida will discuss detection windows for a variety of tests and how the results garnered can best be used. A recording of the presentation and a certificate of attendance will be available 24-48 hours after the completion of the webinar.
Speaker:
Guida Brown earned a bachelor’s degree in Journalism from Marquette University and a master’s degree in Management from Cardinal Stritch University; Guida Brown made the nonprofit sector in Kenosha County her career. She was the Executive Director of the Hope Council on Alcohol & Other Drug Abuse, Inc., for over 13 years, resigning from that position in June 2022. Prior to her tenure at the Hope Council, she worked as the Director of Human Resources and Training at AM Community Credit Union and Executive Director at Women and Children’s Horizons. She is the Principal for Guided By Guida, as well as a Substance Abuse Counselor, Fetal Alcohol Spectrum Disorder trainer, and Intoxicated Driver Program Assessor certified by the State of Wisconsin. She also serves as an adjunct member of the faculty at Concordia University, UW-Parkside, and Gateway Technical College.
A recording of the presentation and a certificate of attendance will be available 24-48 hours after completion.
Click Here to Watch the Webinar

ToxTime: Poster Overview – Prenatal Exposure to Kratom
Please join us for ToxTime with Amy Racines, Research and Development Projects Coordinator at USDTL, for a brief scientific poster overview presentation discussing kratom exposure and detection in newborn umbilical cord tissue.
Amy Racines is the Research and Development Projects Coordinator at USDTL, where she develops and validates new extraction, Immunoassay, LDTD/MS/MS, GC/MS, and LC/MS/MS methods. She holds a Master’s degree in Forensic Science from the University of Florida and has been with UDSTL for over a decade. Amy has papers published in scientific journals related to umbilical cord research and Mass Spectrometry and is a member of many forensic and science-related organizations, including the position of previous President of the Midwest Association of Toxicology and the Therapeutic Drug Monitoring (MATT) and Chicago Chromatography Discussion Group (CCDG).
A recording of the presentation and a certificate of attendance will be available 24-48 hours after completion.
Click Here to Watch the Webinar
Psychedelics are a subclass of hallucinogens that produce changes in perception, mood, and cognitive processes. The most popular psychedelics include lysergic acid diethylamide (LSD), psilocybin, mescaline, and dimethyltryptamine (DMT).
Where Do They Come From
Psilocybin and mescaline are naturally occurring and produced from fungi and the Mexican peyote cactus, respectively.1 LSD, on the other hand, is chemically synthesized. DMT can be chemically synthesized, but most commonly is extracted from a variety of different plants.

Mexican peyote cactus | Sourced by Freepik©Stock
Usage Over Time
Psychedelic use dates back as early as 4000 BC, with evidence of psilocybin and mescaline being used in religious ceremonies.2 DMT was first synthesized in 1931, while LSD was first synthesized in 1943. Both LSD and DMT gained popularity in the 1960s and then in the early 1970s were classified as Schedule 1 drugs.3 Mescaline and psilocybin followed suit and were classified as Schedule 1 drugs in 1971.
After the psychedelics became scheduled, there appeared to be a decrease in usage, but more recently psychedelic use has been on the rise. LSD use rose from 0.55% in 2015 to 0.86% in 2018.4 While overall usage of LSD is still low, that was a 56 percent increase in usage over just 3 years. Psilocybin use has also been on the rise: 8.5% of adults reported usage in 2016, while 9.6% of adults reported usage in 2018.5 Less is known about DMT and mescaline trends, though one study reports mescaline usage has decreased from 2002-2019.6
Getting More Mainstream
We may expect to see a further increase in psychedelic usage due to the increasing popularity of microdosing.7 Microdosing is periodically ingesting minute quantities of psychedelic drugs as a performance-enhancing activity. The levels of psychedelics consumed are so low that a hallucinogenic effect is not experienced, but users report feeling improved mood and focus. There is no scientific literature supporting or refuting the effects of microdosing.

Psilocybin mushrooms, commonly known as magic mushrooms | Sourced by Freepik©Stock
The increased usage of psychedelics is accompanied with mainstream media on the subject. Hulu released a limited series entitled Nine Little Strangers in which the main character, a host at a luxurious wellness retreat in California, microdoses her guests without their knowledge or consent. The creator of the series was reported as stating that he hopes the series will help these types of therapies go mainstream .8 Similarly, Netflix released a movie entitled Have a Nice Trip in which celebrities reminisce about the experiences they had while under the influence of psychedelics. The movie normalizes and makes light of psychedelic usage while failing to mention any of the dangers or negative effects the users may experience. Additionally, just like with marijuana, retail companies have launched apparel and accessories with symbols and designs relating to psychedelics.
Currently, psychedelics are still illegal, but that may soon change. Psilocybin is currently being researched and may receive FDA clearance for the treatment of depression.9 Experts predict the FDA may approve the therapeutic use of psilocybin and MDMA (for PTSD) in as little as 1-2 years. This possible shift in legislation has the potential to change many aspects of the pharmaceutical and drug industry.
References:
- https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/mescaline#:~:text=Mescaline%2C%20which%20is%20derived%20from,to%20psilocin%2C%20the%20active%20moiety.
- https://www.visualcapitalist.com/sp/the-history-of-psychedelics-part-1-of-2/
- https://www.deadiversion.usdoj.gov/drug_chem_info/dmt.pdf
- https://filtermag.org/lsd-increase-research/
- https://akjournals.com/view/journals/2054/5/1/article-p17.xml
- https://www.sciencedirect.com/science/article/pii/S2352853222000499
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6600464/
- https://www.latimes.com/entertainment-arts/tv/story/2021-09-15/nine-perfect-strangers-hulu-psychedelic-psychoactive-jonathan-levine
- https://www.nytimes.com/2022/10/25/health/psychedelic-drug-therapy-patents.html
Sign up here to learn more and receive our newsletter on the latest updates with USDTL.

ToxTime: Ethyl Glucuronide (EtG) in Hair and Nail – A review and Recent Updates
Please join us for ToxTime with Joseph Jones, Ph.D., NRCC-TC, Chief Operating Officer at USDTL, as he presents on what is new with using hair and nail to detect Ethyl Glucuronide (EtG), a long-term ethanol biomarker.
What You’ll Learn
- What is Ethyl Glucuronide (EtG)
- Ethyl Glucuronide (EtG) testing in
- Urine
- Hair
- Nail
- Umbilical Cord Tissue
- A brief overview of previous studies
- And more…
Click Here to Watch the Webinar
When drugs are swallowed, they may be broken down (metabolized) by enzymes and/or absorbed using transporters in cells found in the small intestine. Grapefruit juice can cause problems with these enzymes and transporters, causing too much or too little drug in the body.
Some drugs, like statins used to lower cholesterol, are broken down by enzymes. Grapefruit juice can block the action of these enzymes, increasing the amount of drug in the body and may cause more side effects.

Photo from the U.S. Food & Drug Administration
Other drugs, like Allegra (fexofenadine) used to treat allergies, are moved by transporters into the body’s cells. Grapefruit juice can block the action of transporters, decreasing the amount of drug in the body and may cause the drug to not work as well.
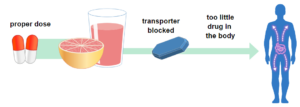
Photo from the U.S. Food & Drug Administration
Grapefruits: Food and Drug Interaction
The Canadian Medical Association Journal (CMAJ) released a review of drugs that interact with Grapefruit, “43 drugs in dangerous ways.”
List of medications that may cause severe side-effects when interacting with grapefruit.
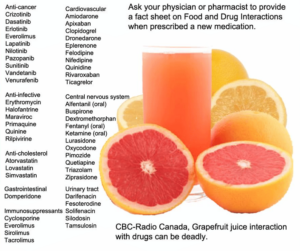
Image by CBC Radio Canada, Information from the Canadian Medical Association Journal
Information collected from:
- https://www.fda.gov/consumers/consumer-updates/grapefruit-juice-and-some-drugs-dont-mix
- https://www.cmaj.ca/content/185/4/309
- https://www.cbc.ca/news/health/grapefruit-juice-interaction-with-drugs-can-be-deadly-1.1253489
- Hair, Nail, and Umbilical Cord Testing for Phenibut, Medetomidine, and Tianeptine
- Umbilical Cord Tissue Testing for SSRIs
- A Comparison of Turnaround-Times for Two Popular Specimen Types Used for Newborn Toxicology: Meconium and Umbilical Cord Tissue
- Using Umbilical Cord Tissue to Identify Prenatal Ethanol Exposure and Co-exposure to Other Commonly Misused Substances
- Toxicology as a Diagnostic Tool to Identify the Misuse of Drugs in the Perinatal Period
- Specimen Delay
- Drug Classes and Neurotransmitters: Amphetamine, Cocaine, and Hallucinogens
- Environmental Exposure Testing for Delta-8 THC, Delta-9 THC, Delta-10 THC, and CBD
- February 2025 (1)
- October 2024 (5)
- March 2024 (1)
- February 2024 (1)
- January 2024 (3)
- December 2023 (1)


